The VIGOUR partners are in the process of preparing the piloting of context-sensitive approaches to integrated care in 15 regions
Integrated care has been a constant topic on the agenda of policy makers and practitioners for decades. As early as 1954, L. E. Burney argued that "comprehensive programmes, such as those designed to bring maximum benefit to persons with chronic diseases ... require the coordination of the efforts of many individuals and agencies".[1] Furthermore, he concluded that a local home care programme implemented at that time had clearly demonstrated "the importance of close integration of clinical, public health and other services if the needs of patients with chronic diseases are to be met to a reasonable degree".[2] There is a widely shared consensus today that integrated care has the potential to improve patient experience and outcomes of care as well as effectiveness of health systems and provider/caregiver experience (known as "quadruple aim"). However, there is still a debate about how the positive potentials generally provided by the concept of integrated care can indeed be realised in practice. All in all, the evidence base that is available today suggests that integrated care is unlikely to evolve as a natural response to emerging care needs in any system of care whether it is planned, or market driven. To put it a little provocatively, it seems as if the debate on integrated care has been going around in circles for almost 70 years. This raises the question why the concept of integrated care is spreading comparatively slowly in practice, despite its generally assumed benefits. The World Health Organisation (WHO), for example, has identified different reasons.[3] To begin with, the absence of a unifying definition has hampered the development of a common understanding what integrated care is or should be about. While it has been possible to identify general principles and core components, it cannot be concluded that one model best supports integrated care. The WHO further highlights that any integrated model development is strongly context-bound and nearly impossible to replicate.
The care authorities participating in the VIGOUR project build on previous efforts to better align existing care delivery processes, albeit in different ways and to different degrees. Against this background, VIGOUR has the objective to take the care authorities from where they currently stand and support them in taking the next step on their specific journey towards integrated care. In doing so, the project aims to effectively support them in progressing the transformation of current care practices towards sustainable models for integrated care. One aspect adding complexity to the implementation of better joined-up care within day-to-day practice concerns the fact that integrated care represents a “nested” concept rather than a pre-defined organisational model of care delivery. The operational implementation of such a concept is, as mentioned, strongly context-bound and can take different forms. Moreover, there is a strong processual element in its implementation, e. g. when it comes to enabling cooperation of different stakeholders across care settings and sectors. Such processes can take different forms depending on given implementation conditions.
Against this background, the care authorities participating in the VIGOUR project are supported by means of a multi-staged process in defining and implementing better joined-up care practices under given framework conditions (Figure 1). Starting from existing care practices, during the initial project phase each VIGOUR pilot site consolidated its initial view on how current service delivery processes might be better integrated. This was followed by a systematic self-assessment of the envisaged integration approach with respect to its appropriateness and feasibility under given framework conditions. The results of this step may require a critical reappraisal of the initially stated integration ambition, e. g. if strongly inhibiting factors or even "roadblocks" were identified at this stage. As a next step, each VIGOUR care authority is now in the process of developing an operational implementation plan as basis for piloting the hitherto developed integration approach under everyday conditions, with a view to preparing further upscaling. While passing through the overall process, each pilot site involves the different stakeholders concerned.
Figure 1 – The multi-staged VIGOUR process
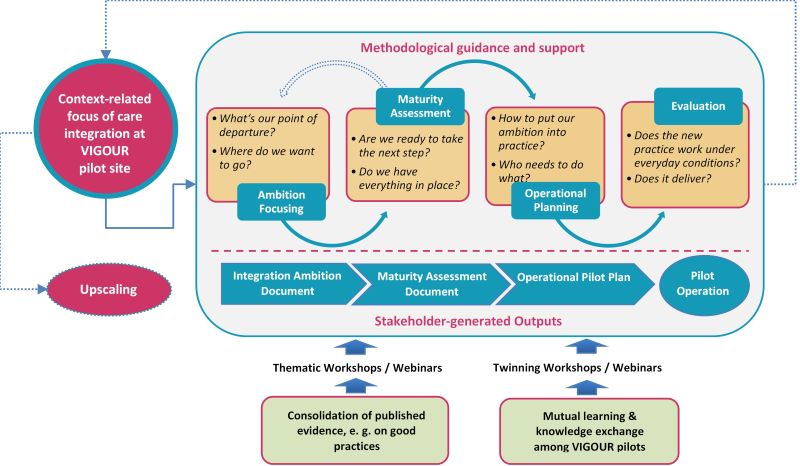
Existing knowledge from published sources is being brought to bear on the VIGOUR process, for the time being by means of webinars and online workshops. Moreover, online workshops are held to enable mutual learning and knowledge exchange between the VIGOUR pilot sites. For instance, pilot sites that are planning to introduce a multidisciplinary needs assessment as part of VIGOUR can benefit from experiences made by others already practicing such an approach. The VIGOUR care authorities will pilot their contextualised approaches towards care integration from mid-2021 until mid-2022. An evaluation workstream will generate evidence on whether the VIGOUR support mechanism sketched above will have delivered the desired outputs by then, with a view to identifying any lessons that can be learned in relation to further scaling-up of integrated care beyond the project’s life cycle.
[1] Burney, L. E. (1954). Community Organization - An Effective Tool. American Journal of Public Health, 44(1), 1–6. doi:10.2105/AJPH.44.1.1 PMID:13114477
[2] Ibidem
[3] WHO Regional Office for Europe: Integrated care models: an overview. Health Services Delivery Programme, Division of Health Systems and Public Health, Working Document, 2016